Blank Wv Peia Prior Authorization PDF Template
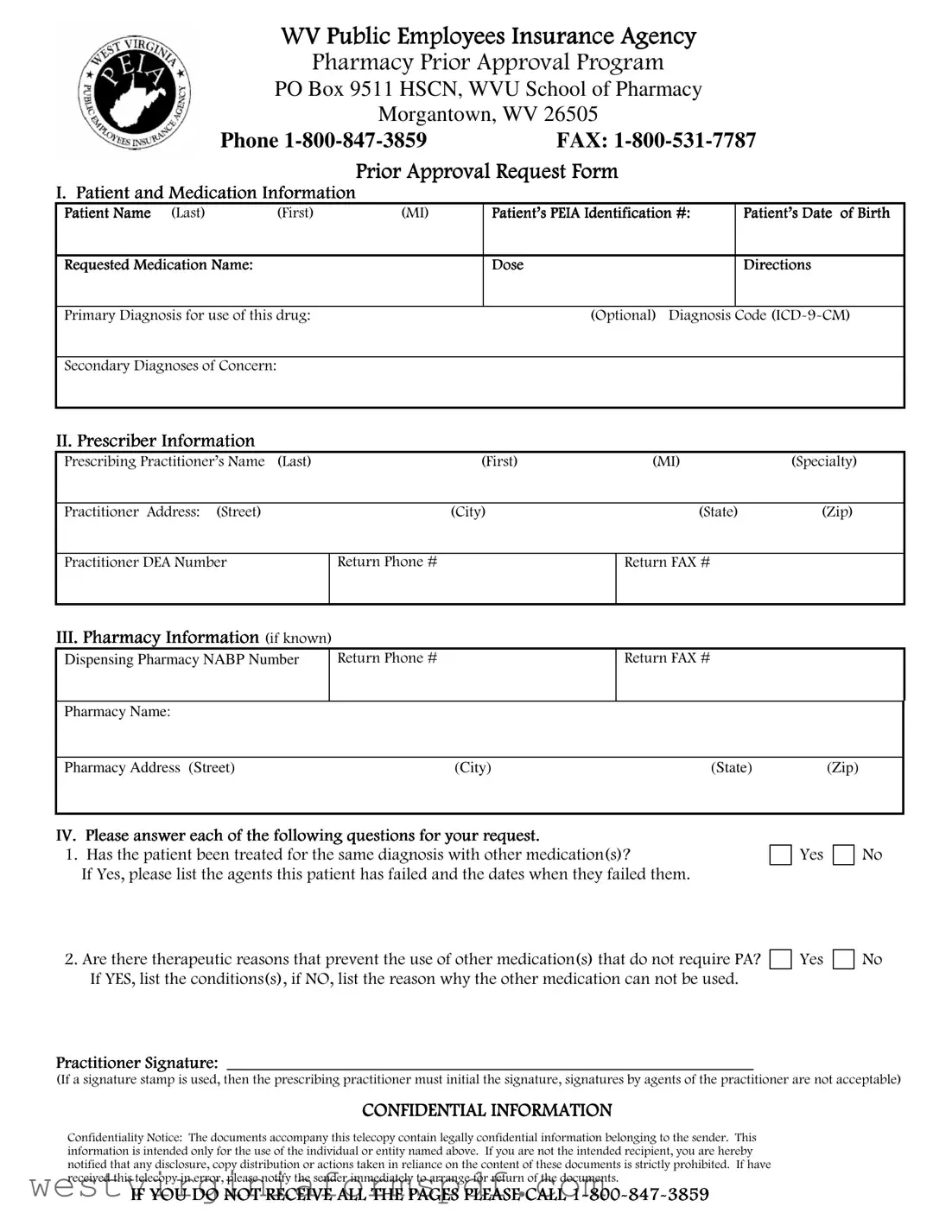
The West Virginia Public Employees Insurance Agency (PEIA) Prior Authorization form plays a crucial role in the healthcare process for state employees and their dependents. This form is essential for obtaining approval for certain medical services, treatments, and medications before they are provided. It serves as a communication tool between healthcare providers, pharmacies, and the PEIA, ensuring that the requested services meet specific criteria for coverage. The form includes necessary details such as the patient's information, the prescribing physician's details, and the requested service or medication. Additionally, it requires the dispensing pharmacy's name and address, along with their NABP number, which helps streamline the authorization process. By completing this form accurately, healthcare providers can facilitate timely access to necessary treatments while ensuring compliance with PEIA guidelines. Understanding the components and requirements of the PEIA Prior Authorization form is vital for both providers and patients, as it ultimately impacts the quality and efficiency of care delivered.
Browse More Forms
West Virginia Cd 3 - The duration for payments should not exceed a maximum of two years.
West Virginia Business Registration - Include the address of the registered office in West Virginia, if there is one.
Once you have decided to embark on your homeschooling journey, it is essential to complete the required documentation to ensure your compliance with state regulations. The Arizona Homeschool Letter of Intent form is a vital part of this process, as it officially informs the state of your intention to homeschool. For further guidance and access to the necessary form, you can visit https://arizonapdf.com/homeschool-letter-of-intent.
Wv Refund - Businesses must provide their tax ID number when submitting the WV/CST-AF2 form.
Form Attributes
| Fact Name | Description |
|---|---|
| Contact Information | The PEIA Prior Authorization form can be submitted via phone at 1-800-847-3859 or fax at 1-800-531-7787. |
| Dispensing Pharmacy Details | The form requires the dispensing pharmacy's NABP number, name, and address, including street, city, state, and zip code. |
| Submission Location | Forms should be sent to PO Box 9511 HSCN, WVU School of Pharmacy, Morgantown, WV 26505. |
| Governing Law | The PEIA Prior Authorization process is governed by West Virginia Code § 5-16-1 et seq. |
Similar forms
The WV PEIA Prior Authorization form is similar to the Medicare Prior Authorization Request form. Both documents serve the purpose of obtaining pre-approval for specific medical services or medications before they are provided to the patient. This ensures that the requested services are covered under the respective insurance plans. The Medicare form requires detailed patient information, including diagnosis codes and the rationale for the requested service, much like the WV PEIA form. Both forms aim to streamline the approval process and ensure that patients receive necessary treatments without unexpected out-of-pocket expenses.
Another document that resembles the WV PEIA Prior Authorization form is the Medicaid Prior Authorization form. This form is used by healthcare providers to request approval for services or medications that may not be automatically covered by Medicaid. Similar to the WV PEIA form, the Medicaid form requires specific patient information and justifications for the requested services. The goal of both forms is to control costs and ensure that patients receive appropriate care while adhering to the insurance guidelines.
Understanding the importance of these forms can greatly enhance the efficiency of healthcare delivery and ensure that patients receive timely and necessary treatments. For those seeking more information on similar legal documents, the TopTemplates.info website offers valuable resources that can help individuals navigate through their options.
The Commercial Insurance Prior Authorization form also shares similarities with the WV PEIA Prior Authorization form. Insurance companies often require healthcare providers to fill out this form to gain approval for treatments, surgeries, or medications. Both forms ask for details about the patient’s condition and the necessity of the proposed treatment. By requiring prior authorization, insurance companies aim to prevent unnecessary procedures and manage healthcare costs effectively, ensuring that patients receive only the most appropriate care.
Lastly, the TRICARE Prior Authorization form is another document that is akin to the WV PEIA Prior Authorization form. TRICARE, which provides health care for military personnel and their dependents, also requires prior authorization for certain services and medications. Like the WV PEIA form, the TRICARE form collects essential patient information and requires a justification for the requested services. Both forms are designed to ensure that treatments align with the insurance policies and that patients receive the necessary care without incurring excessive costs.
FAQ
What is the Wv Peia Prior Authorization form?
The Wv Peia Prior Authorization form is a document required for certain medical services, treatments, or medications under the West Virginia Public Employees Insurance Agency (PEIA). This form helps ensure that the requested service is medically necessary and covered under your insurance plan.
Who needs to fill out the Prior Authorization form?
Typically, healthcare providers or pharmacies complete the Prior Authorization form. Patients may need to provide information or consent, but the responsibility mainly lies with the provider. If you are unsure, contact your healthcare provider for guidance.
What information is needed to complete the form?
To fill out the form, the following information is usually required:
- Patient’s personal details, including name and contact information
- Details about the healthcare provider, including name and contact information
- Specific information about the requested service or medication
- Medical history relevant to the request
- Any supporting documents, such as test results or previous treatment information
How do I submit the Prior Authorization form?
You can submit the completed form via fax or mail. The fax number is 1-800-531-7787, and the mailing address is PO Box 9511, HSCN, WVU School of Pharmacy, Morgantown, WV 26505. Make sure to keep a copy of the submitted form for your records.
How long does it take to get a decision?
The review process for a Prior Authorization request can vary. Generally, you can expect a decision within a few business days. However, some cases may take longer, especially if additional information is needed. It’s best to follow up with your provider if you haven’t received a response within a week.
What if my Prior Authorization request is denied?
If your request is denied, you will receive a notification explaining the reason for the denial. You have the right to appeal the decision. Your healthcare provider can help you navigate the appeals process and may need to provide additional information to support your case.
Documents used along the form
The West Virginia PEIA Prior Authorization form is often accompanied by several other documents that facilitate the approval process for medical services and treatments. Each of these forms serves a specific purpose in ensuring that the necessary information is collected and reviewed efficiently.
- Medical Necessity Form: This document provides detailed information about the patient's medical condition and the necessity of the requested treatment or service. It typically includes clinical data and supporting documentation from the healthcare provider.
- Power of Attorney for a Child Form: For those needing to temporarily delegate parental rights, the comprehensive Power of Attorney for a Child options are crucial for ensuring a child's welfare is managed effectively in your absence.
- Claim Form: Used to submit a request for payment from the insurance provider, this form outlines the services rendered, associated costs, and patient information. It is essential for processing reimbursement.
- Prescription Authorization Form: This form is used when a specific medication requires prior approval from the insurance company. It includes details about the medication, dosage, and the reason for its necessity.
- Patient Consent Form: This document ensures that the patient has given informed consent for the treatment or procedure. It outlines the risks, benefits, and alternatives, and is typically signed by the patient.
- Provider Information Form: This form collects essential details about the healthcare provider, including their qualifications and the services they offer. It helps the insurance company verify the provider's credentials.
- Referral Form: If a patient is being referred to a specialist, this document outlines the reason for the referral and provides relevant medical history. It is often required for certain services to be covered by insurance.
These documents collectively support the prior authorization process, ensuring that all necessary information is available for review. Proper completion and submission of these forms can facilitate timely approvals and enhance patient care.
Dos and Don'ts
When filling out the WV PEIA Prior Authorization form, it’s essential to follow specific guidelines to ensure a smooth process. Here’s a list of things you should and shouldn’t do:
- Do double-check all personal information for accuracy.
- Do provide complete details about the medication or service being requested.
- Do include the prescribing physician’s information.
- Do ensure that the form is signed and dated where required.
- Do keep a copy of the completed form for your records.
- Don't leave any sections blank; fill in all required fields.
- Don't submit the form without verifying the submission method (fax or mail).
- Don't forget to include any supporting documentation if required.
- Don't use abbreviations that may confuse the reviewer.
- Don't assume that your request will be approved without proper justification.