Valid Do Not Resuscitate Order Template for West Virginia State
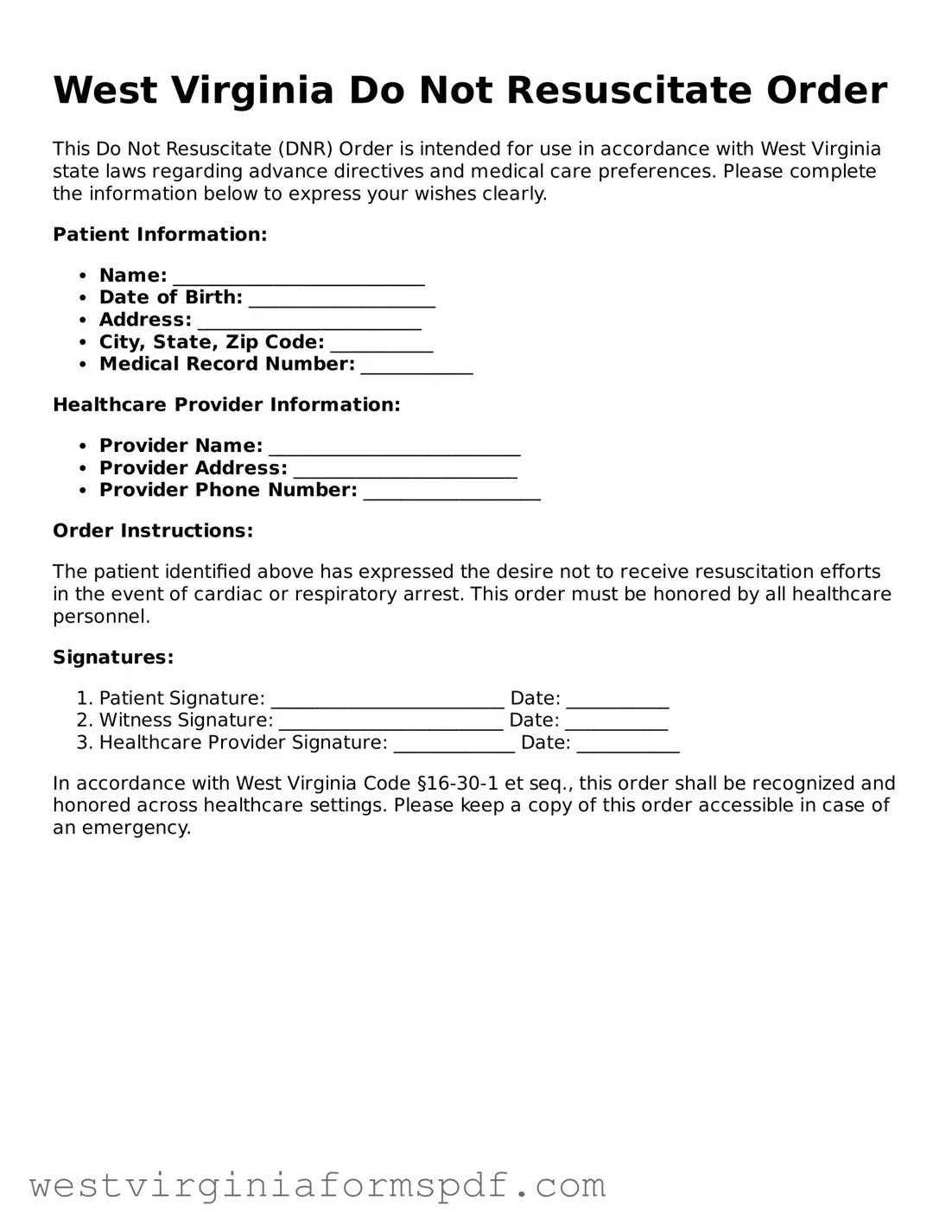
The West Virginia Do Not Resuscitate (DNR) Order form serves as a crucial legal document for individuals wishing to communicate their preferences regarding medical interventions in the event of a life-threatening situation. This form is particularly significant for patients with terminal illnesses or those who wish to avoid aggressive resuscitation efforts that may not align with their values or desired quality of life. It allows individuals to specify their wishes clearly, ensuring that healthcare providers and emergency personnel respect their decisions. The DNR Order must be completed and signed by a licensed physician, and it typically requires the patient’s or their legal representative’s consent. Importantly, the form must be readily accessible to medical personnel, often kept in a visible location within the patient’s home or carried by the individual. Understanding the implications of a DNR Order is essential, as it not only reflects personal choices but also influences the type of care received during critical moments. In West Virginia, this form plays a vital role in facilitating conversations about end-of-life care, empowering individuals to make informed decisions that honor their wishes and promote dignity in their final days.
Consider Other Common Templates for West Virginia
Is a Bill of Sale Enough to Get a Title - This form can also protect buyers in case the seller is later found to have misrepresented the item.
Wv Dmv Title Transfer - Validates the transfer of ownership for future reference.
For those looking to understand the intricacies of property transfer, a well-organized Alabama bill of sale form can be invaluable. Utilizing this document ensures clarity in transactions and protects the interests of both buyers and sellers. For further guidance, you can explore this helpful Alabama bill of sale form resource.
Notice of Intent to Homeschool Wv - It can serve as an affirmation of your child’s right to a tailored education.
File Attributes
| Fact Name | Description |
|---|---|
| Purpose | The West Virginia Do Not Resuscitate (DNR) Order form is used to indicate a patient's wish not to receive cardiopulmonary resuscitation (CPR) in case of cardiac or respiratory arrest. |
| Governing Law | The DNR Order in West Virginia is governed by the West Virginia Code §16-30-1 to §16-30-6. |
| Eligibility | Any adult who is capable of making healthcare decisions can complete a DNR Order form. |
| Signature Requirement | The form must be signed by the patient or their legally authorized representative. |
| Healthcare Provider's Role | A physician must sign the DNR Order to make it valid and recognized by emergency medical services. |
| Emergency Medical Services | Emergency medical personnel are required to honor a valid DNR Order during emergencies. |
| Revocation | The patient or their representative can revoke the DNR Order at any time, verbally or in writing. |
| Form Availability | The DNR Order form is available through healthcare providers and can also be obtained online. |
| Additional Considerations | Patients should discuss their wishes with family and healthcare providers to ensure understanding and compliance. |
Similar forms
The West Virginia Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive, a critical document that outlines an individual’s preferences regarding medical treatment in situations where they cannot communicate their wishes. Like the DNR, an Advance Directive allows patients to express their desires about life-sustaining treatments, including resuscitation efforts. Both documents ensure that a person’s choices are respected, even when they are unable to voice them, thereby providing peace of mind to both patients and their families.
Another document akin to the DNR is the Physician Orders for Life-Sustaining Treatment (POLST) form. The POLST is designed for individuals with serious health conditions and translates their treatment preferences into actionable medical orders. Similar to the DNR, the POLST form is signed by a physician and is intended to guide emergency medical personnel in making decisions about resuscitation and other life-sustaining measures, ensuring that patients receive care aligned with their values and wishes.
The Living Will is yet another document that mirrors the DNR in purpose. A Living Will allows individuals to specify their wishes regarding medical treatment in the event of terminal illness or incapacitation. While the DNR focuses specifically on resuscitation efforts, the Living Will encompasses a broader range of medical decisions, making it a complementary document that works in conjunction with a DNR to provide comprehensive guidance on a patient’s healthcare preferences.
In navigating the complex landscape of healthcare directives, it's crucial to have access to a variety of essential documents. Each form, whether it be a DNR, Living Will, or the Power of Attorney for Healthcare, plays a significant role in ensuring that an individual's healthcare preferences are honored. For those looking for templates to create these important documents, resources like smarttemplates.net offer valuable tools that facilitate the preparation of legally binding forms, making it easier to articulate personal wishes in a healthcare context.
Healthcare Power of Attorney (HCPA) is also similar to the DNR Order form. This document designates a trusted individual to make medical decisions on behalf of someone who is unable to do so. While the DNR specifies the wish to forgo resuscitation, the HCPA allows the appointed agent to make broader healthcare decisions, ensuring that a patient’s overall wishes regarding medical treatment are honored. Together, these documents create a robust framework for patient autonomy in healthcare settings.
In addition to these, the Medical Order for Life-Sustaining Treatment (MOLST) form serves a similar function to the DNR. This document is specifically tailored for patients with serious illnesses and translates their treatment preferences into actionable medical orders. Like the DNR, the MOLST is designed to be easily recognized by healthcare providers, ensuring that patients receive care that aligns with their wishes during critical moments.
The Do Not Intubate (DNI) Order is another document that aligns closely with the DNR. While the DNR explicitly states that a patient does not wish to receive cardiopulmonary resuscitation (CPR), the DNI focuses on the specific refusal of intubation and mechanical ventilation. Both documents reflect a patient’s desire to limit aggressive medical interventions and are often used in conjunction to provide clear guidance to medical teams regarding end-of-life care.
Another related document is the Comfort Care Order, which prioritizes the relief of pain and suffering over aggressive medical interventions. This document complements the DNR by emphasizing palliative care measures rather than curative treatments. Patients who choose a Comfort Care Order often seek to ensure that their final days are spent in dignity and comfort, aligning their care with their personal values.
Lastly, the End-of-Life Care Plan can be viewed as a comprehensive document that encompasses various aspects of a patient’s wishes regarding end-of-life care, including the DNR. This plan may include preferences for pain management, spiritual considerations, and other personal wishes. By integrating the DNR within a broader End-of-Life Care Plan, individuals can ensure that their holistic needs are addressed, providing clarity and guidance to family members and healthcare providers during difficult times.
FAQ
What is a Do Not Resuscitate (DNR) Order in West Virginia?
A Do Not Resuscitate Order (DNR) is a legal document that allows a person to refuse cardiopulmonary resuscitation (CPR) in the event of a medical emergency where their heart stops beating or they stop breathing. In West Virginia, this order is typically used by individuals with serious health conditions who wish to avoid aggressive life-saving measures. It reflects the person's wishes regarding end-of-life care and can provide peace of mind for both the individual and their loved ones.
How do I obtain a DNR Order in West Virginia?
To obtain a DNR Order in West Virginia, follow these steps:
- Consult with your healthcare provider. Discuss your health status and your wishes regarding resuscitation.
- If you decide that a DNR Order is appropriate, your healthcare provider will help you complete the necessary form.
- Once the form is signed by both you and your physician, it becomes legally binding.
- Make sure to keep copies of the DNR Order in accessible locations, such as with your medical records and with family members.
Who can sign a DNR Order?
In West Virginia, a DNR Order can be signed by:
- The individual who wishes to have the DNR Order in place, provided they are of sound mind.
- A legally authorized representative, such as a power of attorney, if the individual is unable to make decisions for themselves.
- A physician who is familiar with the individual's health status and wishes.
It is important that all parties involved understand the implications of the DNR Order and that it reflects the individual's true wishes.
Can a DNR Order be revoked or changed?
Yes, a DNR Order can be revoked or changed at any time. If you decide that you no longer want a DNR Order, simply inform your healthcare provider, and they will assist you in the process of revocation. It is advisable to document this change and inform family members and caregivers to ensure that your current wishes are known. If you wish to modify the order, you will need to complete a new form with your healthcare provider.
Documents used along the form
The West Virginia Do Not Resuscitate (DNR) Order form is an essential document for individuals wishing to outline their preferences regarding medical interventions in emergencies. In addition to the DNR, several other forms and documents can support and clarify a person's healthcare wishes. Below is a list of these important documents.
- Advance Directive: This document allows individuals to specify their healthcare preferences in advance, including decisions about medical treatment and end-of-life care.
- Living Will: A living will outlines specific medical treatments an individual does or does not want if they become unable to communicate their wishes.
- Affidavit of Support: This is an essential document for immigrants, as it ensures financial support from a sponsor. To learn more about this process, refer to the USCIS I-864 form.
- Healthcare Power of Attorney: This form designates a trusted person to make medical decisions on behalf of an individual if they are incapacitated.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that details a patient's preferences for life-sustaining treatments, ensuring those wishes are honored by healthcare providers.
- Medical Release Form: This document allows healthcare providers to share a patient’s medical information with designated individuals, facilitating communication among family and care teams.
- Do Not Hospitalize Order: This order indicates that an individual prefers not to be hospitalized for treatment, aligning with their wishes for end-of-life care.
- Organ Donation Form: This form allows individuals to express their wishes regarding organ donation after death, ensuring their intentions are respected.
Having these documents in place can provide clarity and peace of mind for individuals and their families. They ensure that healthcare preferences are respected and understood, particularly during critical moments.
Dos and Don'ts
When filling out the West Virginia Do Not Resuscitate Order form, it is important to follow specific guidelines to ensure clarity and compliance with legal requirements. Below are six things to consider.
- Do ensure that the form is completed in full, providing all necessary information.
- Do have the form signed by a qualified medical professional, such as a physician.
- Do discuss your wishes with family members and caregivers before completing the form.
- Do keep multiple copies of the signed form in accessible locations.
- Don't use the form if you are not sure about your decision; seek guidance from a healthcare provider.
- Don't forget to review and update the form as your medical situation or wishes change.